Post-Traumatic Stress Disorder (PTSD) is not just a psychological response to a terrifying event—it’s a full-body and brain-level transformation. After trauma, the nervous system and brain don’t just remember what happened—they reorganize themselves to ensure survival. PTSD is more than a memory — it changes the way we experience the world.
Trauma and the Brain: Why PTSD Is More Than Flashbacks
Trauma leaves a distinct imprint on the brain. Key regions are affected in ways that can hijack your sense of safety, time, and connection:
Amygdala: Your internal alarm system. After trauma, it becomes hyperactive, constantly scanning for threats—even when none are present.
Hippocampus: This part of the brain processes time and memory. Trauma can damage or shrink the hippocampus, making past experiences feel like they’re happening in the present.
Prefrontal Cortex: Responsible for decision-making and emotional regulation. Trauma can impair its ability to “put the brakes” on the amygdala, leaving a person reactive, anxious, or overwhelmed.
This breakdown in communication between brain regions explains why PTSD often involves intrusive thoughts, emotional flooding, or complete shutdowns.
PTSD Symptoms: More Than Just Nightmares
People with PTSD may experience a wide range of symptoms that affect daily life:
Flashbacks, nightmares, sleep disturbances
Emotional or somatic numbness, dissociation, feeling detached from yourself, others, or the world around you
Hypervigilance and exaggerated startle responses
Irritability, anger outbursts, or difficulty concentrating
Persistent negative emotional states (i.e. shame, depression, anger, anxiety, hopelessness)
Avoidance of people, places, and things associated with the trauma
These aren’t signs of weakness—they’re evidence that your nervous system is doing everything it can to protect you from future harm. The problem is, it can’t tell the difference between past danger and present safety.
Polyvagal Theory and Neuroception: Your Body’s Inner Surveillance System
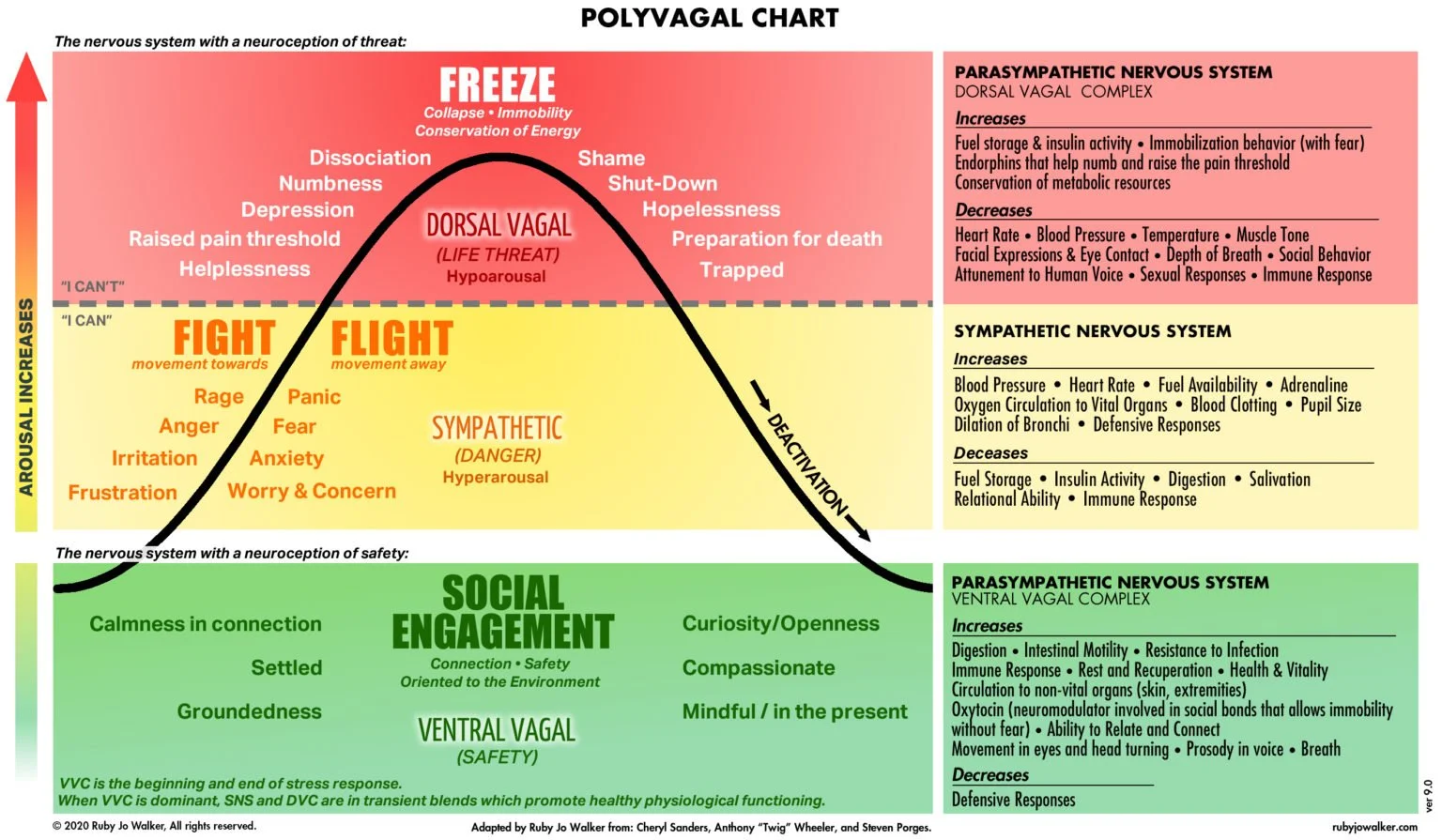
Dr. Stephen Porges' Polyvagal Theory provides a powerful framework for understanding how trauma affects the nervous system. The theory focuses on the vagus nerve, a key part of the autonomic nervous system that governs our responses to safety, danger, and life threat.
Through a subconscious process called neuroception, our body constantly scans for cues in the environment: “Am I safe? Am I in danger?” For those with PTSD, neuroception becomes faulty—reading danger in neutral or even safe settings. This leads to constant cycles of:
Fight or Flight: Anxiety, panic, restlessness, anger
Freeze or Shutdown: Dissociation, numbness, fatigue, disconnection, withdrawal
It’s not in your head. It’s in your body. Because traumatic experiences bias neuroception towards protection which leads to a mismatch between autonomic states and actual levels of safety or danger. This mismatch activates protective strategies which keep you from accurately sensing safety and inhibiting defense responses, or identifying danger and activating protective responses.
This is why trauma survivors often feel hijacked by their own physiology. Even in calm environments, their bodies are still preparing for or responding to real or perceived threat.
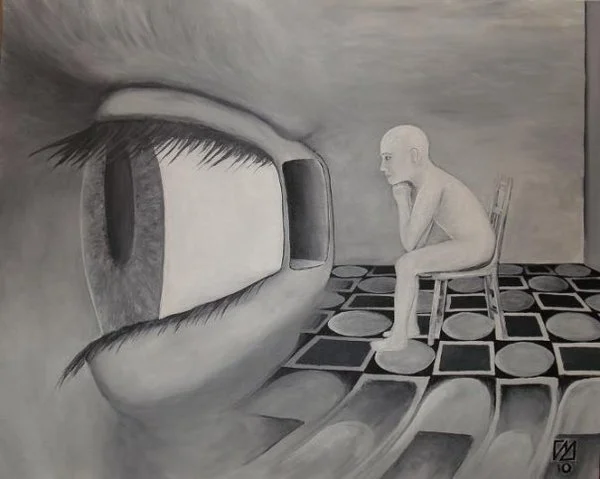
PTSD is More Than a Memory—It’s a Shift in Perception
Living with PTSD can feel like having a faulty alarm system in your brain and body—one that never shuts off. The world feels unsafe, people seem untrustworthy, and even your own thoughts and sensations feel threatening.
But here’s the truth: You are not broken. You are adapting. And adaptation means there’s potential for healing.
Healing is Possible: EMDR and Professional Support
If you recognize yourself in these symptoms, the most important step is to seek help. PTSD doesn’t resolve on its own, and white-knuckling your way through it is not a long-term strategy.
EMDR therapy is a research-backed, body-informed treatment that works directly with how trauma is stored in the brain. It helps restore emotional balance, quiet the alarm bells in your nervous system, and bring the past into its rightful place—the past.
PTSD changes the way you experience the world—but it doesn’t have to define your future.
With support, it’s possible to rewire your nervous system, reconnect with your body, and reclaim your life.
Ready to take the first step?
If you or a loved one identifies with these symptoms, reach out to a licensed trauma therapist.
Explore whether EMDR therapy might be the right fit for your recovery.
Share your story—your experience may offer hope to someone who feels alone.
***
Weston Zink is a Licensed Professional Counselor and Licensed Addictions Counselor in the State of Colorado, and the founder of Breakthrough Recovery of Colorado, where he specializes in helping individuals navigate the complex challenges of trauma, addiction, and recovery. With over a decade of clinical experience in trauma and addictions counseling, Weston brings a grounded, compassionate, and evidence-based approach to healing work, guiding clients toward lasting change and self-discovery.
Weston is an EMDR Certified Therapist, Consultant-in-Training, and member of EMDRIA since 2022 who’s working to heal traumatized people and communities at home and abroad.
Known for his ability to tackle tough topics with honesty and heart, Weston blends professional insight with a down-to-earth style that resonates with those ready to do the deep work. When he’s not in session, you’ll likely find him hiking Colorado’s rugged trails, volunteering with Rampart Search & Rescue, reading and writing about the human experience, or enjoying meaningful time with family and friends.
If you need help overcoming the challenges of trauma, addiction, and/or other mental health issues, or are interested in learning more on how you can strengthen your recovery journey, please contact us for a free consultation at: https://breakthroughrecoveryco.com/schedule-therapy-consultation-appointment.